FG To Absorb 28,000 Health Workers Affected By USAID Freeze — Minister
The freeze in billions of dollars in global funding for the United States’ health and education projects in countries of the world including Nigeria continues to dominate global discussions.

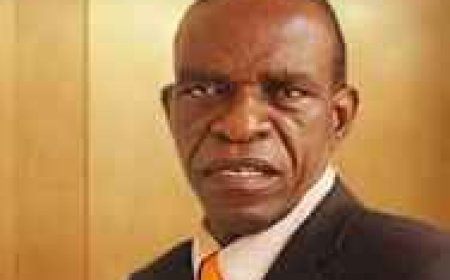
Channels Television ---------- The freeze in billions of dollars in global funding for the United States’ health and education projects in countries of the world including Nigeria continues to dominate global discussions. There have been palpable fears on the continental scene that the decision of the Donald Trump presidency to halt the United States Agency for International Development, USAID, will reverse the compounded gains achieved in the global fight and campaign against diseases and infections such as malaria, tuberculosis, Human Immunodeficiency Virus, HIV, and its advanced stage, the Acquired Immuno-deficiency Syndrome, AIDS,. On Channels Television’s Hard Copy programme, Prof Ali Pate, Nigeria’s Coordinating Minister of Health and Social Welfare, speaks on Nigeria’s preparedness to manage the impact of America’s aid cut on interventions in the health sector. He also speaks on the fate of 28,000 Nigerian health workers previously paid by the aborted American programme.
Excerpts:
What would you say the primary challenge has been with Nigeria’s health sector?
The fundamental issue is that we have not invested seriously in our health infrastructure, in our health human resources, and equipment. We have not come together as a nation to build a National Health System. The Federal Government had its parts, states had their part, and local governments too. Some pulled more than others. The government’s revenue, as a portion of our GDP, has been very low.
So, of the little that the government collects, it had prioritised health lower, education lower, but this president, in his Renewed Hope Agenda, had put human capital as a core and we have seen a deliberate effort to invest more in health and service delivery. We have begun to see the impact of those slowly happening but it will take time for a system that has spent years without the required infrastructure, equipment and human resources to supply chain consumables.
It’s a system and that system will take time to get to the point where people will see a much larger transformation which is possible. When folks think about the UK or the US Healthcare System where many of our compatriots go. Those systems spend a large chunk of their resources for health. The UK spends more than $4,000 per capita in health. Here, we’re talking about $120 per capita, total, of which public financing is about 30% of that. So, you can look at the disparity. The United States, for instance, about $4,000 per capita. Healthcare is not cheap. Quality healthcare is not cheap. You have to invest in it. We as a country had not invested in it and yet we had been asking for the highest quality health. The few elite afford it, they go out but domestically we have not invested.
Now, we have seen that change in the last 18 months with a deliberate effort to improve the investments and to allocate the Investments where it matters — the foundation, the primary healthcare, the higher-level health infrastructure, the cancer infrastructure that we’re rebuilding, the teaching hospitals, the equipment, the human resources, the expansion of the training, the regulatory oversight, the harmony in the sector and the production of the commodities that we need to deliver, whether it’s antibiotic. Can you believe that more than 70% of our drugs, we import with foreign exchange that we didn’t have? So, if we can flip it over time. 99% of our medical devices, we import them.
Now, if we flip that over time, that is not going to take place overnight but we have to be on that path. What we’re trying to do is to change a trajectory and we’re beginning to do that. First, it requires political will and we have seen it. The president unveiled the Renewal Investment Initiative and we saw 36 state governors join the Federal Government and sign a contract.
We’ve seen deliberate efforts to mobilise resources to invest in health. Just last week, the Federal Executive Council approved almost a billion dollars in terms of financing for the programme. That is a significant resource that states will implement. It’s a programme for results that will deliver better but it will take time. We can have the health system that we desire.
Complaining on the sidelines and thinking that things will not change or things are so bad is not going to get us there. We are acting in that direction and I believe many leaders are keying into that because all the 36 state governors have now expressed interest to join the Federal Government in this journey. Our private sector actors, the hospitals, the providers, and the pharmaceutical industry should also rise up. This will make our healthcare system serve Nigerians and potentially even serve other parts of our continent.
Our total health spend in Nigeria, the total health exposure: 30% is public, 70% is private. So, the component of overseas development assistance for health is not the largest chunk of our health expenditure.
How significant is overseas assistance?
It has been significant. We’re a very large country and while we talk about the total health expenditure overall and a 70% that is domestic private and the 30% that comprises the public as well as the overseas development assistance, I will say about $67 per capita is what the external development assistance is about. Now, that is about $67 per capita if you multiply by 200 million Nigerians, that’s about the figure.
The US government has been a key component for a very long time but it’s not the only one. There are others — the UK government and other development partners contribute. Some are technical partners; WHO and the UN, they contribute and we appreciate it, not only about the money that folks bring but some bring technical expertise and we appreciate it. The US government has contributed significantly, for instance, in HIV, TB or malaria but much of those resources are not channeled through government systems; they’re channeled through implementing partners outside government and that is the risk, the vulnerability and we’re seeing that unfold now.
Are we at risk? I mean how vulnerable are we?
For us, we are not complaining; we are full of appreciation to the US government for the contribution they have made: the American people have contributed in taking care of more than 1.3 million Nigerians on anti-viral therapies, tuberculosis, malaria, maternal and child health conditions. The change in US government policy is the determination of the American people. We can’t complain. What we have determined is that we are primarily responsible for the health of our population and we are going to work towards exiting the dependency on external assistance, particularly in view of the transition that the US government has made.
While appreciating what the US has done, we know that there may be other ways that the partnership between Nigeria and the US government will continue. We spent time to analyse the quantum and the support that had been provided outside government and did a bottom costing, if we were to take that as the public sector and we now have completed that assessment of what it will take for HIV, tuberculosis and malaria. As you recall at the Federal Executive Council, the president set up a cabinet committee involving the minister of finance budget, myself, the minister of state for defense, and the governor’s forum to think of that transition so that the government as a responsible government owns this problem.
It’s our population and to ensure that we don’t lose grounds on that. We’ve assessed what is on the ground and we have determined a quantum of resources. We will identify where to source that so that we buy the commodities and buy them in such a way that we encourage those who are producing them to come and produce in Nigeria as well because that is sustainable in the long run, to look at the supply chain how do we manage it in our context.
We may be a poor country but we are a capable country and we are determined to own up that responsibility. Now, if others step in and support us, we appreciate it but we are not begging for it and we also will live within what we have but we have the responsibility on us as leaders to ensure that our population gets the care they need. The Federal government is going to do its part. For states, we expect that they will also step in because there are many things that happen at the state level on HIV, TB or malaria. There are health workers, 28,000 of them who were been paid through US government support. While it has been appreciated, those health workers are Nigerians. We have to find ways to transit them.
Our approach, long before the change in US policy has been towards increasing national ownership, increasing domestic resources, improving our healthcare value chain and producing what we use, strengthening our resilience through surveillance, laboratory systems so that we deal with infectious diseases. We never really absorbed ourselves of the responsibility for taking care of Nigerians who require government support. Health is right and it has a value inherently and is key to the future prosperity of our country.
So, the pivot that the US government has met in a way found us where we had already been moving in that direction and it’s just about raising the additional resources to be able to cope and we are confident that Nigeria can be able to cope. It may not be able to buy the most expensive versions of the medications that the US dollars buy but with the resources that we have I believe that we can find those who have those medications, generic as they may be, but with the quality that is needed that we buy and distribute to our population and we want to safeguard the progress that has been made on HIV.
The electricity situation, for instance in the University College Hospital, Ibadan, has remained intractable. It’s over 100 days now and we’re still counting. This is a well-known hospital in darkness.
This has been a story for several years of accumulated debt to the Ibadan Disco. The hospital was disconnected and we stepped in to help the hospital The chief medical director, over the last three months, has done an incredibly good job of transiting to off-grid power, solarise many of the wards, theatres and others. He developed a mechanism whereby there are hours when the hospital uses diesel for theatres to operate so it’s not as if the hospital wasn’t functioning; it was functioning within certain bounds and using off-grid resources to power the hospital. I can show you the pictures of UCH at night three days ago with light; it’s not as if they are in darkness.
The UCH power was connected to the University of Ibadan and there are private entities within the university so the University College Hospital was paying for a bill of what it consumes as well as others including residences that are within that perimeter. So, disentangling that is necessary. How can the hospital bear the burden including residences of those who are not necessarily working in the hospital?
If you go to UCH, if you call the CMD, he will tell you the hospital functions, the theatres function. There are patients. I can show you live recordings of those of the hospital just three days ago.
In the 2025 budget, not only UCH but almost all our hospitals. We’re working through the Rural Electrification Agency to solarise them so that we use alternative power sources to power our facilities because the cost of diesel is encroaching on their internally generated revenue.
What's Your Reaction?